4 tips for a low FODMAP Christmas Dinner
/Blog reproduced with permission from Glenda Bishop. Glenda is a Registered Nutritionist, wellness coach, neuroscientist and educator.
When I was growing up, Christmas was a favourite time of year. As a kid, it was more about the presents. But as I got older, it was more about the food. In Australia, Christmas is in summer, which means lots of summer stone fruits. It also means many sweet treats using dried fruit, such as plum pudding, fruit cake and fruit mince pies.
But these types of foods don’t work on a low FODMAP diet and more than a bite or two of the old Christmas favourites will lead to a very unhappy tummy. So that’s the downside... having to change the way you do things and what you can eat. The upside is it’s possible to come out ofChristmas day without your belly feeling like it’s going to explode.
To help you have a low FODMAP Christmas dinner, especially when you aren’t making it yourself, I’ve put together a few tips so you can keep your IBS under control and still enjoy your day.
Tip 1: Watch your overall FODMAP intake over the day
One of the biggest challenges with Christmas dinner is there’s multiple parts to the meal... appetisers, mains and dessert, along with alcohol and extra nibbles, all of which are eaten over a few hours.
So while a single course may be low FODMAP, eating several courses in rapid succession could easily push you over your FODMAP threshold.
Here’s some strategies for managing your overall FODMAP intake during the meal (and the day):
Be ultra careful with your FODMAP intake on Christmas morning and the day before. The effect of FODMAPs adds up between meals, so keeping your FODMAP intake very low prior to Christmas dinner gives you more wiggle room for the potential overload that’s coming.
Keep a close eye on your portion sizes across the whole meal to prevent overloading from an additive effect. For instance, if you’re going to be eating stuffing made from a low FODMAP sourdough bread, it’s probably a good idea to avoid eating extra slices of sourdough bread during the meal. This is easiest to do if you know what’s being served in all courses before you eat anything–so ask if you’re unsure. Then you’ll know what to eat and what to skip.
Don’t be afraid to ask questions about ingredients in the foods. The best way to manage your FODMAP intake is to always know which meal choices are high or low in FODMAPs.
Avoid grazing on nibbles and appetisers. Odds are these will add FODMAPs to your overall load that you don’t really need. Besides, the actual meal should be enough to fill you up unless you’re going to be there for a very extended period.
Avoid alcohol or other drinks that will add to your FODMAP intake and instead save the FODMAP load for food. Keep in mind that alcohol, even if low FODMAP, may aggravate your IBS anyway. So go easy on the alcohol and only drink it during the meal.
Of course you may decide that something is worth eating even if it’s high FODMAP. After all, it is Christmas. That of course is your choice and only you can weigh up the pros and cons of triggering your IBS. But if you do this, remember it was your doing and try accepting the consequences gracefully.
Tip 2: Roast meat and veggies can be a winner, but watch out for seasonings and stuffings.
A roast is exceptionally common for Christmas dinner. While some countries favour turkey, in Australia we’re more likely to have roast chicken, pork (with lots of crackling), leg of ham, or even lamb. Served up with lots of roast veggies of course.
The good thing about roasts is that so long as they aren’t prepped with garlic or onion, they’re normally an excellent choice for a low FODMAP diet. But even if the cook does rub garlic on the outside for extra flavour, most people should be okay to eat a serve of meat from the inside of the roast, provided that the roast is cut carefully to prevent spreading the garlic around. But do remember that FODMAPs are water soluble, so a little may make its way into the inside of the roast.
A better scenario is for the meat to be prepped without fresh garlic, so try talking to the host ahead of time to see if they can accommodate your needs (see the bonus tips for more info). And if they do want to add garlic flavour, suggest they use garlic-infused oil, which is beautiful rubbed onto the surface of a roast before cooking.
If your roast has stuffing, there’s very little chance it will be low FODMAP unless specially prepared. That’s because most stuffing recipes contains onion, garlic and bread, and sometimes dried fruit too. Of course, you could make stuffing with the green tops of spring onions, garlic-infused olive oil, anda low FODMAP bread, but if someone else is preparing the roast, this may not be an option.
When it comes to roast veggies, again it depends on how they’re prepared. If the host was planning to use garlic or onion for flavour, ask them to pop your veggies into a separate pan before cooking them.
Tip 3: Be very careful with gravies and sauces.
As a general rule, most gravies and sauces aren’t going to be low FODMAP because most will have garlic or onion.So unless you know for sure that they’re safe, you may want to skip them altogether.
There are a few exceptions though:
Cranberry sauce, if made with whole cranberries and sugar, doesn’t have added FODMAPs. But you’ll need to limit your portion size to about 1 tbsp. You can use cranberry sauce with chicken, turkey or ham.
Mint sauce and mint jelly are low FODMAP options, although they’re generally served with lamb and may not suit your Christmas dinner.
Gravy can be made without onion or garlic, especially if it’s made at home from scratch from pan drippings. But only if no onion or garlic was added to the roast because the fructans would have dripped into the pan while roasting and so will end up in any gravy made from the gravy.
Mustard is an excellent choice for ham, but do check there’s no garlic, onion or honey in the mustard. I prefer the Maille brand of mustard - Dijon or wholegrain - both of which are low FODMAP.
If there’s seafood on the menu, common for many Australian Christmasses, you can make a low FODMAP Thousand Island Dressing from mayo, chives, red-wine vinegar, sugar, dijon mustard, Worcestershire sauce (Lea & Perrins is gluten-free and Monash has found that Worstershire sauce is low in FODMAPs despite having onion and garlic in it. If you are not willing to risk it, however, you can definitely forgo this ingredient), paprika, salt and pepper.
Tip 4: Unless dessert is specially made, it’s probably off-limits, except for fresh fruit.
When it comes to FODMAPs, desserts are particularly tricky to navigate. There are very few regular desserts that won’t be high FODMAP. Regular plum pudding with custard, fruit cake and mince pies are off the list, as is a standard trifle. There are some possibilities though:
Custard is suitable if made with lactose-free milk or a low FODMAP non-dairy alternative.
Pavlova can be a good choice if the topping is appropriate, but you can also scrape off the topping and eat the pav instead. But do watch if it’s store-bought because there could be hidden FODMAPs.
Low FODMAP fresh fruit can also be a good choice, perhaps with some low FODMAP nuts if there’s any lying around from the bowls of nibbles. Or with some hard cheeses and crackers, if you can tolerate dairy.
An easier way around the dessert conundrum is to take something along with you that you know is low FODMAP and that everyone else will enjoy too. A lovely option is this beautiful Spicy Gingerbread Cake with Orange Glaze that’s perfectly suited to a Christmas dinner.
Bonus Tips: Speak to the host ahead of time to see if they can make some adjustments or if you can bring something along.
I’ve mentioned it a few times in this article already, but it’s worth repeating this as a separate tip. Talking to the host before the big day gives you a chance to explain your needs and see what can be done to help you. Most people will be willing to make changes for you.
The best way to approach this is to explain that you have a range of food intolerances and that you’re not asking them to change everything for you, but instead you want to be sure that there’s something that will be safe for you. I know that ideally it would be great if you could eat anything that’s served, but sometimes you need to accept that this isn’t going to happen.
I then ask what they’re planning on serving and make some suggestions based on my biggest intolerances. For me that means focussing on garlic, onion, dairy and large amounts of wheat. Then based on what they’re willing to adjust (or not), I make suggestions on what I can bring along to make things easier. That might include bread, sauce, dessert, dips, a salad, etc..
Lastly, remember that you’re there for the company. So as long as you don’t end up starving, it’s not the end of the world if you have to miss out on some things.
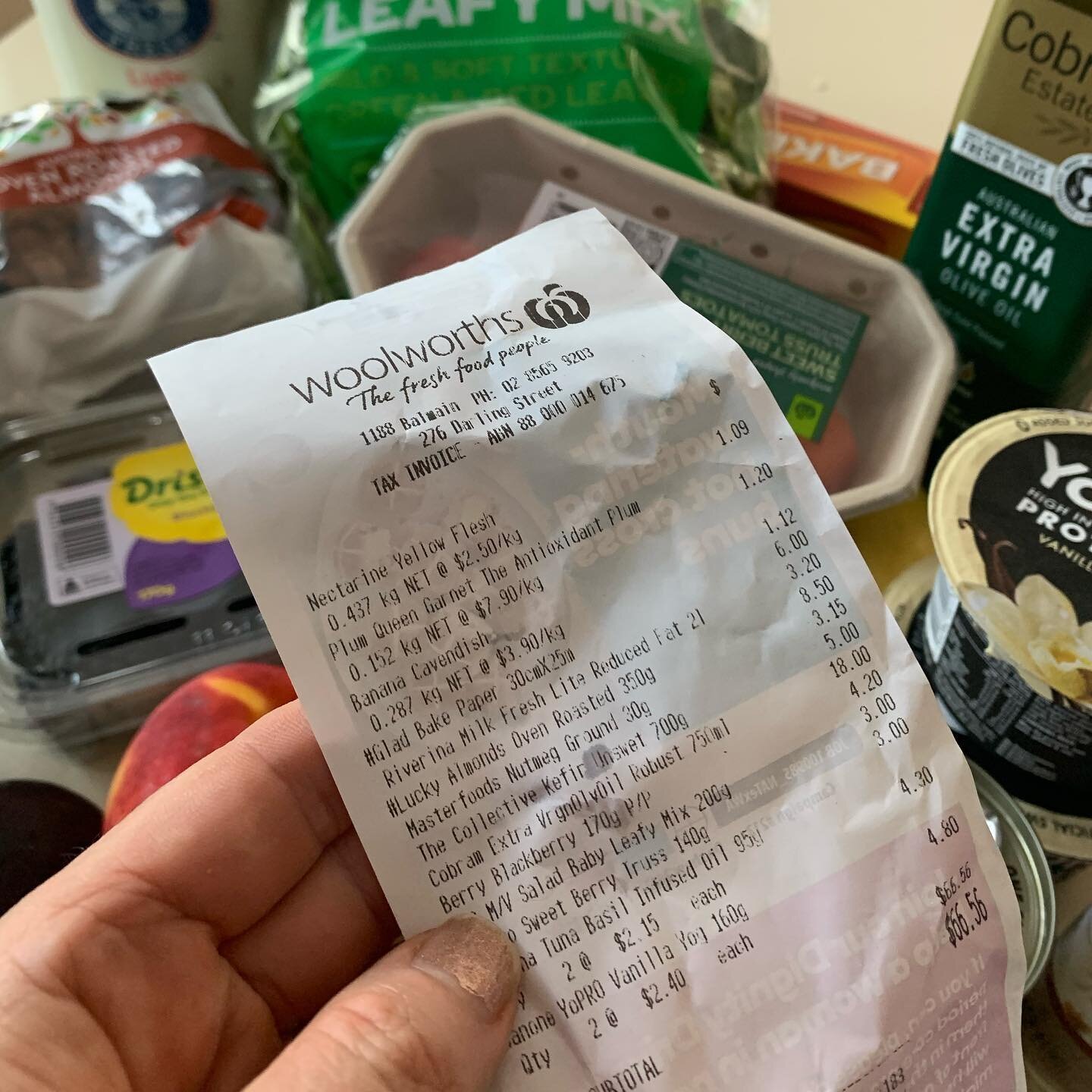
Rachel is a university qualified Clinical Nutritionist based in Balmain. She is also the busy working mum of two teenagers, so is practical and realistic with her advice . Rachel offers private consultations to improve your family's health and well-being. You can find her on Facebook and Instagram for more healthy tips and tricks.
If you'd like help implementing a low FODMAP diet I can help you. Find out more about my services here. If you’re after more delicious low FODMAP recipes go here.
If you're an athlete looking to manage a sensitive gut during training, read this.
If you're interested in gut health, head here.